CSF loss : epidemiology, symptoms, dynamic exploration and treatment
CSF loss: epidemiology, symptoms, dynamic exploration, and treatment
This session will be presented by Dr. Federico Cagnazzo, accompanied by Dr. Waleed Brinjikji. They will share their experiences on the diagnosis and endovascular management of the rising star of neurointervention, “spontaneous intracranial hypotension (SIH)”.
First point: Think about SIH
SIH is a debilitating, mysterious disease due to loss of CSF at the spinal level. It has various symptoms, and the most common symptom is orthostatic headache, which is characterized by having or worsening of headache in the upright position [1].
Some other common symptoms are: [2]
•Nausea and/or vomiting, neck pain and/or stiffness, hearing problems
• Tinnitus, vertigo, dizziness, back pain, movement disorders
• Reduced level of consciousness, diplopia, photophobia
The variety of symptoms and lack of a typical presentation lead to misdiagnosis and underdiagnosis of SIH. The estimated incidence of SIH is nearly as frequent as ruptured aneurysms, which is around 5 in 100000 [1].
Practical points to overcome the underdiagnosis of SIH
• “We need to educate the physicians about SIH, and physicians that see these patients are primary physicians or headache physicians.” (Adnan Siddiqui)
• “About 1/3-1/4 of patients present with only sensorineural hearing loss or Meniere’s disease phenomenon.” (Waleed Brinjikji) So educating and collaborating with otolaryngologists to evaluate these patients for SIH is essential.
Second point: Make the diagnosis
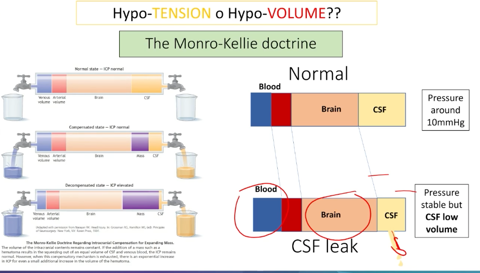
This excellent image from Dr. Cagnazzo’s presentation demonstrates the basic pathophysiology of the SIH. The Monro-Kellie doctrine explains that total volumes of CSF, brain tissue and cerebral blood are constant. If we lose CSF due to a leak or a venous fistula, brain tissue and cerebral blood will compensate it by increasing their volumes. Although there is less volume of CSF, the CSF pressure is usually normal [3].
When we consider the basic pathophysiology of the SIH, it is not hard to imagine the typical imaging findings:
•Brain tissue will expand and increase its volume – expansion and sagging of the brain stem and cerebellar tonsils.
• Cerebral blood volume will increase- engorgement of the cerebral sinuses.
• Loss of CSF–effacement of CSF-filled cerebral cisterns
• Prolonged intracranial hypotension may lead to edema in the dura, which makes the gadolinium enhance -classic pachymeningial (dural) enhancement. Also, the traction effect on cerebral veins may cause subdural haemorrhage [4]
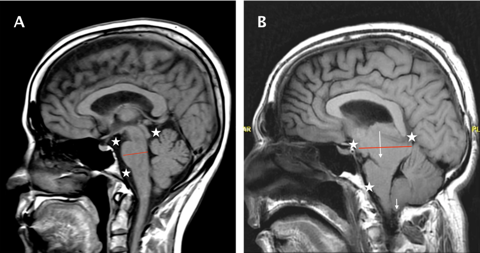
Demonstrative image from Dr. Cagnazzo’s presentation shows the brain MRI of a normal patient (A) and a patient with SIH (B). Effacement of cerebral cisterns(stars), expansion of the brain stem(red transverse line) and sagging of the brain stem and cerebellar tonsils (white arrows) showed.
Although imaging findings are essential for diagnosis, we should be aware that up to %20 of the patients have a normal brain MRI [1]. Bern scoring system was developed by evaluating typical brain MRI findings in SIH patients confirmed to have a CSF leak [5].
|
Three major criteria (2 points each) |
Three minor criteria (1 point each) |
|
-Pachymeningieal enhancement -Engorgement of venous sinus -Effacement of suprasellar cistern ≤4 mm |
-Subdural fluid collection -Effacement of the prepontine cistern ≤ 5 mm -Mamillopontine distance ≤6.5 mm |
Third point: Find the etiology/leak
Type 1 leaks consist of a dural tear. Its subdived in T1a ventral CSF leaks(%96), T1b posterolateral CSF leaks(%4) [6].
•Spinal longitudinal extradural fluid (SLEC) exists in almost all ventral dural tears, and T2W-fat sat images are important to show it and differentiate it from epidural fat.
• Bony abnormalities and calcifications are also common in ventral dural tears.
• Dynamic-prone CT myelography (CTM) is essential imaging to localize the level of tear for guiding the surgery.
Type 2 leaks are characterized by meningeal diverticula and are subdivided into simple and complex types [6].
• SLEC may accompany
• Dynamic lateral decubitus digital subtraction myelography (DSM) and/or CTM are essential for the diagnosis [7]
“I personally don't believe that Type 2 leak is a thing; I think most of them have a CSF-venous fistula” (Waleed Brinjikji)
Type 3 leaks are CSF-venous fistulas.
• Most are located on the right side and in the thoracic region.
• Dynamic lateral decubitus DSM and/or CTM are essential for the diagnosis [7]. Please watch the session for practical details of the imaging technique.
• Renal excretion of contrast after CT myelography is %100 specific finding of CSF- venous fistula [8].
• On day 1, perform the right side DSM, day 2, left side DSM and day 3 embolization session if you find it.
Fourth point: Treat the lesion
CSF leaks that can be treated by endovascular approach are CSF-venous fistulas.
• The aim is to selectively catheterize the paraspinal vein that drains the fistula detected in DSM and embolize it with Onyx [9].
• Puncture the right common femoral vein (generally preferred).
• Advance the 6 Fr Benchmark catheter to the Azygos vein (for thoracal fistulas) over a 5 Fr diagnostic catheter. (For lumbar fistulas ascending lumbar vein and for cervical fistulas vertebral vein)
• After guiding catheter placement, catheterize the paraspinal vein with Headway Duo or Scepter XC microcatheter.
• Perform the venogram and confirm the location, then embolize with Onyx.
• Filling the epidural space with Onyx during embolization is usually cause no problem.
• Please watch the session for practical details of the treatment technique.
Further Reading
[1] T. Dobrocky et al., “Spontaneous intracranial hypotension: searching for the CSF leak,”
Lancet Neurol, vol. 21, no. 4, pp. 369–380, Apr. 2022, doi: 10.1016/S1474-
4422(21)00423-3.
[2] L. D’Antona et al., “Clinical Presentation, Investigation Findings, and Treatment Outcomes of Spontaneous Intracranial Hypotension Syndrome: A Systematic Review and Meta- analysis,” JAMA Neurol, vol. 78, no. 3, pp. 329–337, Mar. 2021, doi: 10.1001/JAMANEUROL.2020.4799.
[3] P. G. Kranz, T. P. Tanpitukpongse, K. R. Choudhury, T. J. Amrhein, and L. Gray, “How common is normal cerebrospinal fluid pressure in spontaneous intracranial hypotension?,” Cephalalgia, vol. 36, no. 13, pp. 1209–1217, Nov. 2016, doi: 10.1177/0333102415623071/ASSET/IMAGES/LARGE/10.1177_0333102415623071- FIG4.JPEG.
[4] E. X. Sun, J. Shi, and J. C. Mandell, Core Radiology: A Visual Approach to Diagnostic Imaging. Cambridge University Press, 2021. [Online]. Available: https://books.google.com.tr/books?id=AgZDEAAAQBAJ
[5] T. Dobrocky et al., “Assessing Spinal Cerebrospinal Fluid Leaks in Spontaneous Intracranial Hypotension With a Scoring System Based on Brain Magnetic Resonance Imaging Findings,” JAMA Neurol, vol. 76, no. 5, pp. 580–587, May 2019, doi: 10.1001/JAMANEUROL.2018.4921.
[6] W. Schievink, M. Maya, S. Jean-Pierre, M. Nuño, R. Prasad, and F. Moser, “A classification system of spontaneous spinal CSF leaks,” Neurology, vol. 87, pp. 673–679, 2016.
[7] N. Luetzen, P. Dovi-Akue, C. Fung, J. Beck, and H. Urbach, “Spontaneous intracranial hypotension: diagnostic and therapeutic workup,” Neuroradiology, vol. 63, no. 11, p. 1765, Nov. 2021, doi: 10.1007/S00234-021-02766-Z.
[8] S. Behbahani, J. Raseman, H. Orlowski, A. Sharma, and R. Eldaya, “Renal Excretion of Contrast on CT Myelography: A Specific Marker of CSF Leak,” AJNR Am J Neuroradiol, vol. 41, no. 2, pp. 351–356, Feb. 2020, doi: 10.3174/AJNR.A6393.
[9] W. Brinjikji et al., “Clinical and imaging outcomes of cerebrospinal fluid-venous fistula embolization,” J Neurointerv Surg, vol. 14, no. 10, 2022, doi: 10.1136/NEURINTSURG- 2021-018466.